Christmas 2022 was a terribly traumatic ordeal for Denise Devoto, who had pneumonia which progressed to sepsis.
After a challenging recovery journey, she is sharing what happened to her in an effort to raise awareness and encourage others to Just Ask: Could it be sepsis?
Denise woke up in the middle of the night on 9th December 2022 with a sharp pain in the right-hand side of her ribcage, and in her lungs. By the 15th of December, she thought it had developed into a cough and cold. She had a job interview that morning, which she dragged herself to coughing and spluttering. On 17th December she woke up with a really bad coughing fit and a pain that ripped through her ribs.
The next day, she went to the walk-in centre, who thought she had a blood clot on her lungs, so they sent her to the Northern General Hospital in Sheffield. Denise said: “It was the week before Christmas and there were lots of cases of strep A in the walk-in centre waiting to be seen. When I got to the hospital, A&E was absolutely rammed full of people. I spent 9 hours there and eventually saw a doctor, and I tested positive with flu.”
Doctors thought she’d strained a muscle from all the coughing; they sent her home with co-codamol for the pain and told her to come back the next day to collect a prescription for Tamiflu. But by the Monday, Denise had started vomiting phlegm – not just coughing it up. She said: “I thought, ‘I know that’s not right. I must have developed a chest infection as well’.”
She rang her GP the following morning, who prescribed some antibiotics, which Denise’s husband collected on his way home from work. But by later that afternoon, she started to feel really breathless and had turned grey and her lips were blue. She rang her GP again who advised that she needed to call an ambulance. Her husband rang 999, and paramedics arrived within 10 minutes. Although her oxygen levels were right, paramedics knew something else was going on, so took her to hospital. Denise said: “They took me in and when they got there it was chaos. There were 10-12 ambulances queuing outside. But one of the paramedics went into resus and said you need to make space. So, they did get me in as quickly as they possibly could.”
Denise was put on oxygen, and then started having very bad diarrhoea. After a few hours the Doctors decided to transfer her to the Infectious Diseases Unit at the Hallamshire Hospital. Within an hour of being there, they had started her on antibiotics and fluids and pain relief, as well as the oxygen. They had also started her on nebulizing meds to clear her chest. Denise said:
“Quite often people describe the feeling of feeling like they’re going to die when they start with sepsis. It did truly feel like that’s what was going to happen.”
“But I didn’t know at that time that it was sepsis. My diarrhoea continued to get worse and worse, to the point where I couldn’t stop passing watery bowel movements.”
By 4am, doctors recommended that Denise’s husband come in to try and help keep her calm. Doctors from the critical care unit told her that she had pneumonia and had gone into septic shock, as her organs had been struggling for oxygen. They were particularly worried about her kidneys and liver because her blood pressure had plummeted. Denise said: “They didn’t actually move me to intensive care at that point, but I was very much on their radar in case I deteriorated any further and needed intensive nursing. Thankfully I avoided that. During the first 24 hours in hospital, I had eight different Doctors looking after me and they said I was the most poorly patient on the ward at the time.”
Although she avoided going into ICU, Denise did struggle with hallucinations – including seeing loved ones that she had lost. She said: “At one point I’d actually got my mum, my dad and my brother sat around my bed talking to me, which really freaked me out because they’ve all been dead a long time. I was really quite traumatized that I could see them, and I was hearing all sorts of different voices, and music playing that wasn’t playing. The Doctors advised it could be the medication they had put me on or the infection, or maybe even a combination of both that were causing my hallucinations.”
After receiving vast amounts of intravenous fluids, Denise retained a lot of fluid, and it caused her to gain about two and a half stones in weight. As her kidneys had been damaged by the sepsis, the Doctors had to wait to see if the fluid would shift on its own as giving her diuretic medication could have made her kidneys worse.
By Christmas day, her breathing worsened along with the pain in her lungs and ribs. Denise said: “I think because of being in hospital over the Christmas period, there were just not the number of doctors in hospital, so I felt like I went a little bit off the radar. The Wednesday before New Year’s Eve, one Doctor thought I was well enough to be discharged and said my breathing difficulties were down to me having panic attacks. Thankfully my husband was able to advocate for me and refused to let me be discharged. Eventually on the Friday before New Years Eve, they sent me for a CT scan and X-rays, which showed a large bilateral pleural effusion in my lungs, and that was why I was struggling to breathe. I’d also fractured three ribs from coughing and had a partially collapsed right lung.”
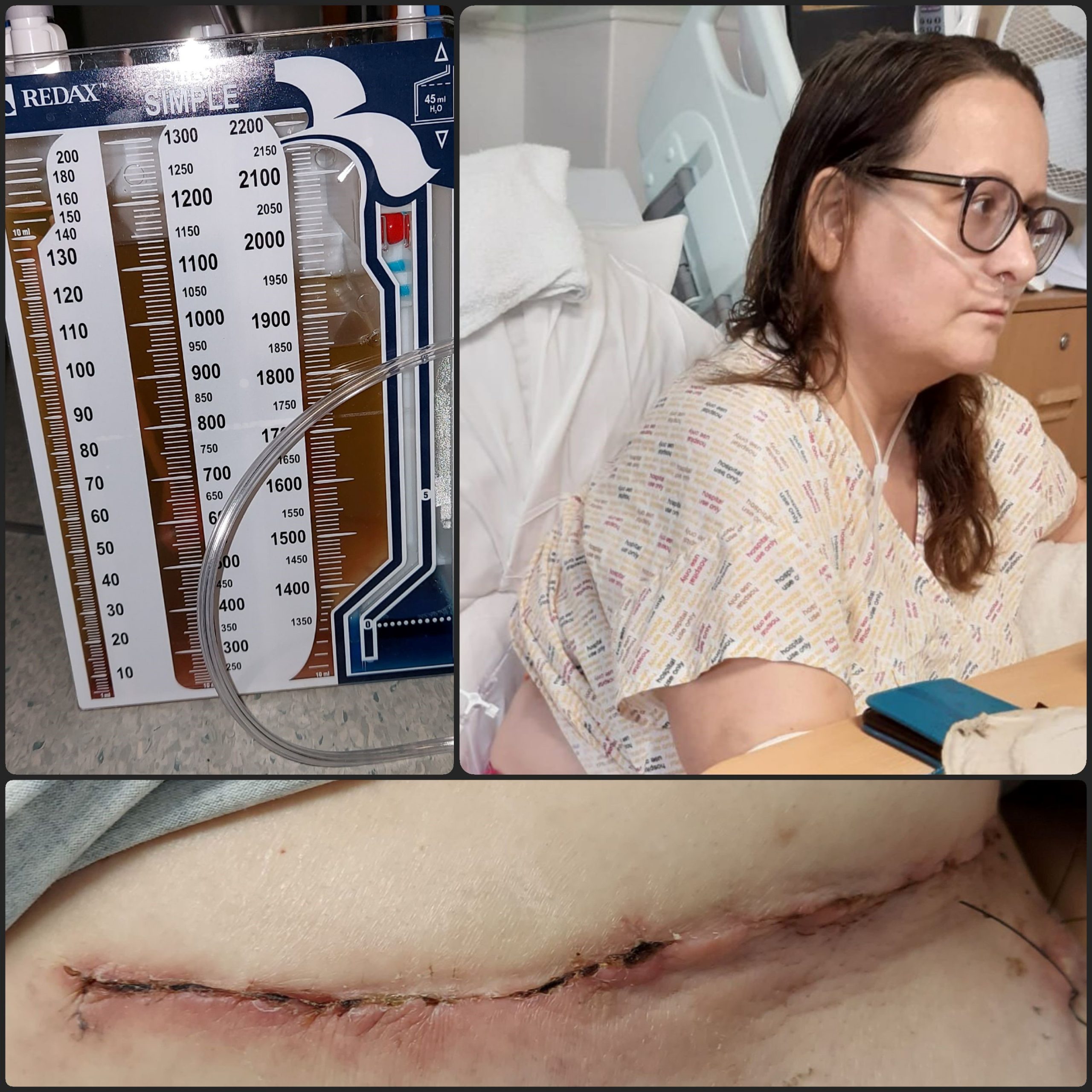
She was then transferred back to the Northern General Hospital, where she had a lung drain fitted to initially clear a litre of fluid. Denise remained in hospital for a two-week period, where they drained four litres of fluid from her lungs during that time. But the infection still hadn’t shifted; a further CT scan showed that the infection had solidified in places on Denise’s lungs and developed into what is called an empyema. Doctors originally thought that they would be able to remove it via keyhole surgery, but the thoracic surgeon couldn’t get the camera through the infection, so Denise had to have a full decortication of her lungs to remove the infection. Denise now has a 12-inch scar on her back from this. They removed ten large pieces of the infection, with the surgeon describing it as being like ‘peeling an orange’.
Denise had a blood transfusion after her operation and was kept intubated for the first 24 hours following the surgery to help her lungs recover, before spending a further five days on the intensive care unit. She said: “Even though I was really quite poorly myself, part of what was traumatic was the really poorly people that were around me. Especially when those poor people went into cardiac arrest, and I was aware of what was happening around me.”
Denise spent the last five days of her hospital stay on the thoracic ward, before being discharged on 24th January 2023 after five weeks in hospital. She later picked up norovirus, which made her recovery even more difficult. A few weeks after being discharged, Denise found the UK Sepsis Trust’s Facebook support group through a friend who also had, had sepsis – having been given no information about sepsis before leaving hospital. She said:
“Once I was admitted to the group and I could see all these posts, it all sort of started to make sense to me and the realisation of what I’d been through.”
She also spoke to a UKST Support Nurse. Denise said: “I spoke with Emma. She was really supportive, really understanding, and she suggested that when I had an appointment with my GP next that I gave him the information about the UK Sepsis Trust, etc. and then just see once he’d got that information, what further support he could provide to me going forward.”
Denise’s GP familiarised himself with sepsis, before coming to see her for a home visit. She said: “He had obviously made himself really familiar before he came to visit me at home and was really empathetic and understanding and validated how I was feeling. I can’t fault my GP’s care. He kept in touch with me every two weeks and just made sure that I’d be fit to return to work, etc. He has also ensured I had the necessary follow up appointments with the hospital for such as how my voice has been affected from it all.”
Her sepsis experience and subsequent recovery also had a huge impact on her husband. Denise said: “I felt bad for the impact it was having on my husband because he was having to do everything and he took time off work, unpaid, to care for me and, doing all the housework and just everything that I couldn’t do.”

“I felt very debilitated by it all and spent the first couple of months sleeping about 18 hours a day to recover.”
Denise joined a UKST sepsis support group, to try and make sense of common sepsis after effects, such as hair loss, and voice changes (as a consequence of having been intubated and the trauma caused to her vocal cords from such a bad cough from the pneumonia). “I thought as much support as my husband, family and my friends can give me, there’s actually nothing like speaking to all the people that have been through the similar thing that you have. Just to have that peer support and know that people truly get it and understand is invaluable. I lost about 50% of my hair a couple of months after being discharged, which was really upsetting, and my voice hasn’t returned to normal (it completely went for several weeks in hospital). I am currently waiting to see if I need surgery to remove nodules that have formed on my vocal cords and also waiting for follow up appointments with the hospital as my eye sight has deteriorated since my sepsis. I’ve never had great eyesight, but my optician thinks the floaters that have developed in one of my eyes and how my peripheral vision has deteriorated is related to having sepsis. I also still have scar tissue pain in my wound, have been left with a persistent cough and struggle with fatigue,” said Denise. “I would say to anybody that’s thinking of joining an online or a face-to-face meeting that the UK Sepsis Trust provide, if there’s one in their area, do go along, give it a try. You don’t have to say anything if you don’t want to. You can just sit and listen.“
As well as physical side effects, Denise struggled with leaving the house and socialising initially, due to feeling fatigued, and the fear of reinfection. Her mental health also suffered due to spending so long in hospital and also at home due to how poorly she had been. But having a P!nk concert in Sunderland on the 10th June this year was a milestone that she worked towards. Denise said: “It was the most amazing weekend with the girls possible and I’m so proud of myself that I managed to get there. I paid for it the week after from fatigue. But it was worth it! I think just having that goal is what kept me going, thinking, “Well, I’ve got to get back to work before I do that.”
Sheffield City Council employee Denise began a phased return to work on 9th May, with the support of her very supportive manager and her team. Working from home allows Denise to nap if she needs to on her lunch break, to combat fatigue, and she is hoping to access funding via the Access to Work Scheme which will provide transportation to the office to prevent the risk of reinfection on public transport, especially during the winter period. She said: “It makes a huge difference if you’ve got an employer that understands and is empathetic to what you’ve gone through, and what you’ll continue to go through as well.”
Denise’s advice to her coworkers, and anyone reading this is: “Make yourself aware of the symptoms of sepsis, but also be aware that just because they’re the symptoms that are listed, there might be other things as well that might cause you to have concerns. Never be afraid to challenge anyone in the medical profession. If you’ve got a gut feeling that something really isn’t right, then challenge them. Because with hindsight, what I should have done when I was in A&E on the Sunday evening, is said, ‘I’m too poorly, I really feel this is more than just flu.’”
As well as encouraging people to get their flu jabs, Denise also wants hospitals to do more to equip patients that have had sepsis with information – which is exactly what UKST is doing with its hospital pilot project. She said: “If hospitals do start to give out more information about sepsis to people that have been affected, even if it’s just a leaflet or a card to link them to the Sepsis Trust, it would make a huge difference to a lot of people. I know it would have done to me and many others I have spoken to on the UK Sepsis Trust Facebook group.”
Make sure you know the signs:





