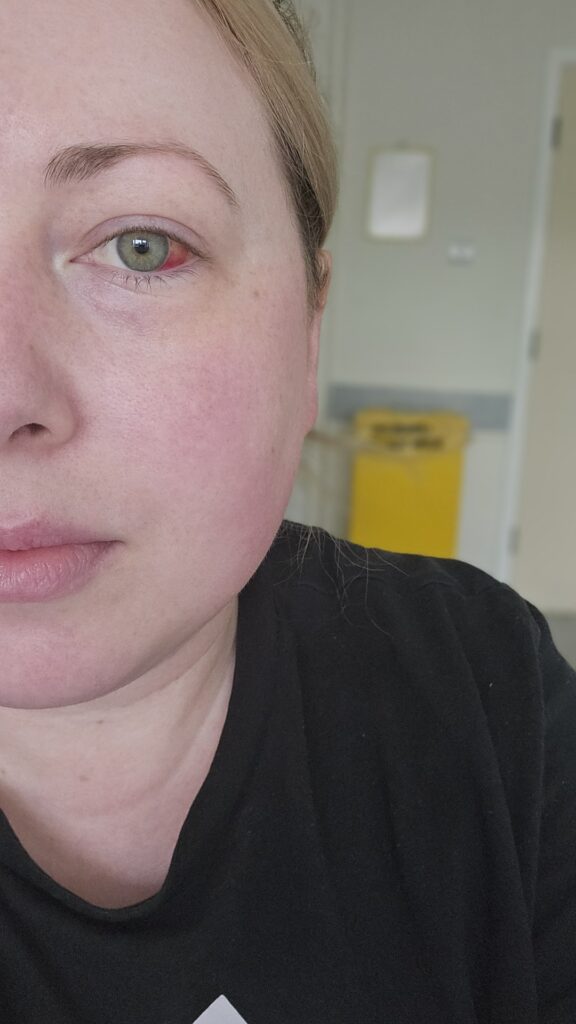
Sarah James developed life-threatening sepsis from a chest infection after returning from a holiday to San Francisco. She was rushed to A&E with a 40°C fever, severe breathlessness and dangerously low blood pressure.
Now recovered, Sarah wants others to act quickly if illness lingers or worsens, and to know that Post-Sepsis Syndrome is real and can last long after hospital discharge.
Sarah, 36, from West Yorkshire first felt unwell shortly after returning from a trip to San Francisco.
“I put it down to the plane, there were a few people coughing on board,” she said. “After three weeks I still felt ill. I had tightness in my chest, a cough, I felt very tired and was beginning to feel hot.”
Her GP initially diagnosed a chest infection that had led to a secondary infection, prescribing antibiotics and steroid tablets.
“A week later I felt no better,” Sarah said. “I was breathless, had a 40 °C fever, was experiencing chills with severe muscle shaking, and my heart felt like it was racing.”
When she returned to the GP surgery the doctor immediately recognised the danger.
“After checking my blood pressure and seeing it was low, my GP said, ‘I’m worried it may be sepsis,’ and referred me straight to A&E,” Sarah said.
Hospital tests confirmed the diagnosis, and Sarah was admitted to an acute illness ward.
“I just felt very unwell,” she said. “I had no energy, my asthma made breathing really difficult, and my whole body felt under attack. But I’d been trying to push through.”
Sarah’s hospital stay was challenging.
“I was moved wards three times, often around midnight,” she said. “Having to fill out forms and answer questions at ridiculous hours when I was so unwell didn’t help my recovery.”
After discharge, the difficulties continued, as Sarah wasn’t given much aftercare and didn’t know about Post Sepsis Syndrome until she did her own research.
Sarah said. “I experienced hair loss, trouble sleeping, anxiety and brain fog. It slowly eased over six to nine months, but I had to research it all myself.”
Before her illness Sarah knew little about sepsis.
“I’d only heard of septic shock from things like tampons being left in too long,” she said. “If I could go back, I’d tell myself not to wait so long. If I hadn’t delayed, my chest infection might not have turned into something nastier.”
She now urges others to trust their instincts.
“Be self-aware, because sepsis can happen at any age,” Sarah said. “If you’re not improving, don’t think it will just go away. And listen to the people around you – my partner Michael was the one who said, ‘This isn’t okay, you need to call your GP or 111.’ That probably saved my life. I’ve always been the type of person who doesn’t like taking time off or calling in sick to work when I’m unwell. But my partner knew this wasn’t a typical illness for me, through his persistence I’m here today. I’ll always be thankful to him for that.”





