Today, on World Sepsis Day 2024, we’re urging the government to re-prioritise sepsis, ensuring it is treated with the same urgency and resources as strokes and heart attacks, after a new YouGov survey commissioned by UKST has detected record public awareness levels.
According to the nationally representative omnibus survey, an impressive 94% of the 2,087 respondents are aware of sepsis, with 91% recognising it as a medical emergency. This is a marked increase from 76% in 2019 and baseline levels 27% in 2012, showcasing the effectiveness of the charity’s ongoing awareness campaigns.
These figures surpass public awareness levels in several other developed countries, including the United States (65%), Australia (50%), and Germany (74%).*
Dr Ron Daniels, UKST’s Founder & Joint CEO, said: “While we’re encouraged by the high level of public awareness in the UK, which exceeds that of most other developed nations, awareness alone is not enough. It is now the responsibility of our government to ensure our health service is equipped to respond effectively and reliably to people with sepsis in of all ages. By matching this awareness with action, we can save lives and improve outcomes for the thousands of people affected by sepsis each year.”
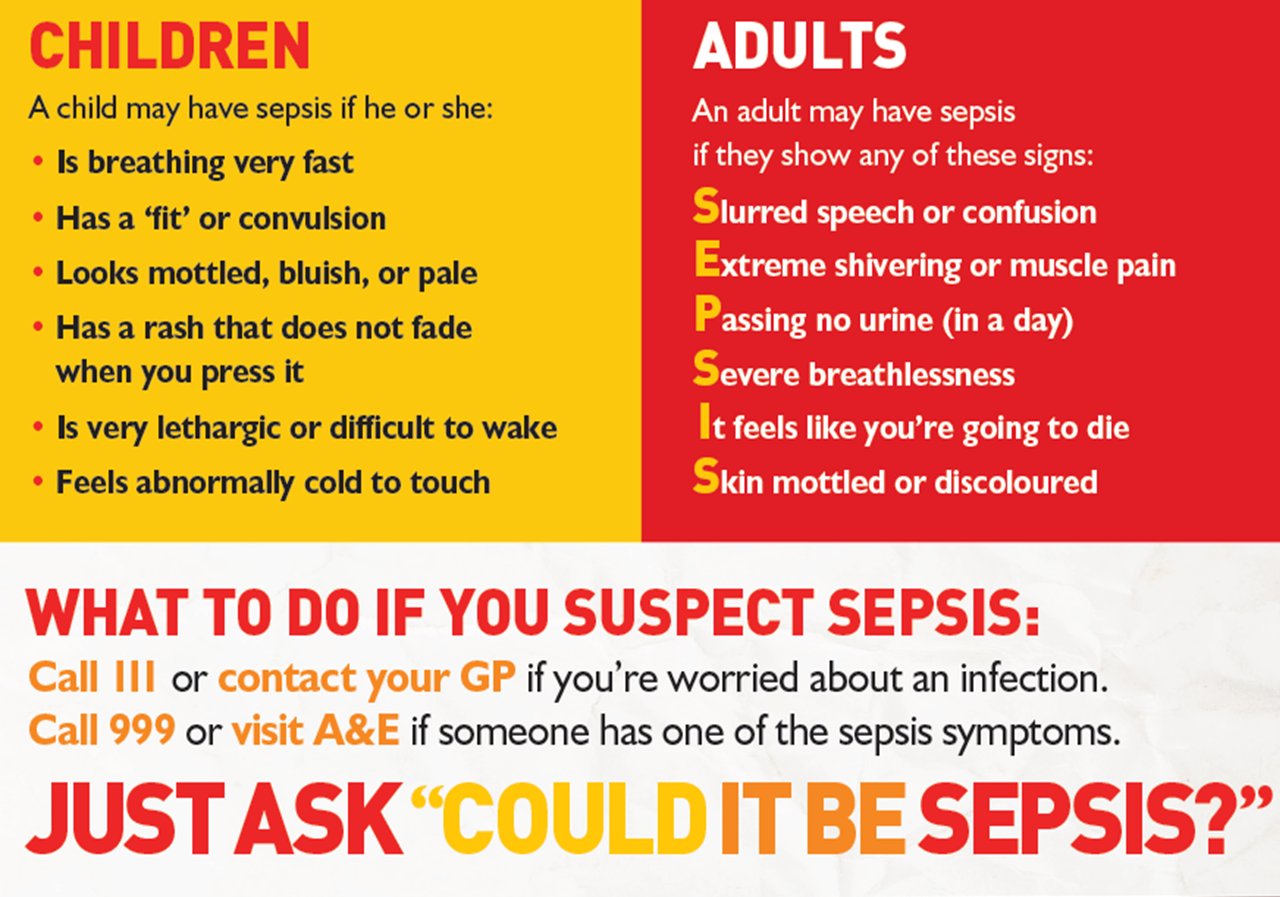
While awareness that sepsis is a medical emergency has encouragingly increased, the same YouGov survey found that there is still limited understanding of the various symptoms, which differ for adults and children; only 31% of respondents said they would be confident recognising if they or someone else might have sepsis.
The YouGov survey also revealed that 45% of respondents either know someone affected by sepsis or have been personally affected by the condition. This statistic underscores the pervasive impact of sepsis on individuals and families across the UK, with 245,000 affected each year and 48,000 losing their lives to this often ‘killer’ condition.
Despite this encouraging improvement in public awareness, there remains a pressing need to enhance sepsis care within our health services. One family that knows this only too well is medically trained professionals Duaa Sidahmed and Mohammed Hassan, who lost their son Yousef to sepsis in February 2023, just after his first birthday, despite following the charity’s guidance to ‘Just Ask: Could it be Sepsis?’.
Mohammed said: “I was dismissed when I asked the doctor if it could be sepsis; so record public awareness levels are encouraging, but awareness only goes so far. Health professionals need to listen to families that raise their concerns and follow the sepsis care pathway, to prevent tragedies like the one our family has experienced.”
Duaa said: “We can’t find the words that can describe the pain of losing Yousef, or the love we have for him. We were over consumed by anger, but with the support of our family and friends, and reaching out to the UK Sepsis Trust as well, that feeling is a bit better now, but we had many moments of shock and denial. Sometimes I just can’t believe that Yousef is really gone, and I find myself calling his name or singing his favourite songs. But every day is a hard day. Everything seems to be triggering and I think we’re just trying our best to cope and accept that grief will forever be a part of us, and this is our way now to show love and remember Yousef.”
The UK Sepsis Trust believes that decline in sepsis outcomes is related to a de-prioritisation of sepsis in the wake of the Covid-19 pandemic.
Dr Daniels said: “During the Covid-19 pandemic, attention to sepsis care understandably diminished, leading to gaps in timely and effective treatment. As we emerge from the pandemic, it’s crucial to refocus our efforts on this life-threatening but often treatable condition. We’re calling on the government to commission clear and efficient pathways within the NHS, supported by integrated care boards, to ensure that suspected sepsis is taken seriously – every time – in Accident & Emergency (A&E) departments nationwide.”
Even when sepsis outcomes do not result in tragic loss of life, many survivors and their families continue to suffer from long-term health issues and challenges.
Mandy Moores, mother of identical twins Tilly and Lucy, can see the impact a childhood sepsis experience following chicken pox has had on Tilly’s cognitive development, with Tilly struggling at school compared to her academically able sister. Mandy said: “Our family perhaps is uniquely placed to evidence the long-lasting effects of sepsis; while we’re enormously grateful for the care that Tilly received, we agree that more needs to be done to provide support and education to survivors and their families, so they know what to expect after leaving hospital.”
UKST provides free, Support Nurse-led services to survivors, many of whom find their ability to function is impacted by Post Sepsis Syndrome (PSS) – with symptoms reported by sepsis survivors including fatigue (80%), anxiety (53%), and trouble concentrating (47%). 37% report difficulty performing tasks they could previously, while 34% suffer with Post Traumatic Stress Disorder (PTSD). It’s easy to see how this affects peoples’ ability to work.**
But UKST found that 83% survivors were not told about PSS by healthcare professionals, and 68% of survivors and 64% of caregivers of survivors, weren’t given information about support resources and services after sepsis.
Craig Mackinlay, who was dubbed the ‘bionic MP’ after surviving sepsis resulted in a quadruple amputation, said: “I know first-hand the devastating effects sepsis can have. It is unacceptable that so many survivors are left to struggle without the support they need; we can’t have a postcode lottery when it comes to health. The government must step up and ensure that everyone who has battled sepsis receives the care and resources necessary to not only survive the condition but go on to rebuild their lives.”
To help improve sepsis outcomes, The UK Sepsis Trust is calling for the government to:
- Measure and publish performance data on the sepsis care pathway. Reliable data are needed to understand the quality of NHS sepsis care, identify opportunities for improvement and provide targeted support where needed.
- Empower frontline decision-making with better integration of rapid diagnostics. There is no single test to diagnose sepsis, but diagnostics help doctors make important decisions about the types of treatment to use. Diagnostic tests are typically done in centralised laboratories, which means clinicians have to wait for the results. Time is of the essence when treating sepsis, so health professionals need access to fast and reliable tests to reduce preventable deaths.
- Raise awareness of the signs and symptoms of sepsis and signpost rehabilitation services to reduce pressures on the NHS. Empowering the public to ‘Just ask “Could it be sepsis?” can help save lives, and ensuring survivors have access to ongoing care and support will help keep them well and out of hospital.
Ensuring comprehensive and consistent sepsis care across the UK
We recognise that health is a devolved matter in the UK. Therefore, while this call to action is directed primarily at NHS England, we also expect the health services in Scotland, Wales, and Northern Ireland to adopt similar measures.
Consistent and comprehensive sepsis care must be a priority across the entire UK to ensure that all patients receive the timely and effective treatment they deserve.
References
* 2023 YouGov data published by Sepsis Alliance, available online
Eitze, S., Fleischmann-Struzek, C., Betsch, C., & Reinhart, K. (2018). Determinants of sepsis knowledge: a representative
survey of the elderly population in Germany. Critical Care, 22(1). https://doi.org/10.1186/s13054-018-2208-5
**Extrapolated from Prescott HC, Angus D. Enhancing recovery from sepsis- a review. JAMA 2018; 319(1):62-75
Iwashyna TJ, Ely EW et al. Long-term cognitive impairment and functional disability among survivors of severe sepsis.
JAMA 2010 304(16):1787-94
*** UKST collected data from 744 caregivers of sepsis survivors as part of a Support survey issued in August 2024



