Aaron Speer was diagnosed as a Type 1 Diabetic in 2017, which radically changed his life, setting up a chain of events which would leave him to develop sepsis three times.
He is bravely sharing his experience as a now clean former intravenous (IV) drug user to make others aware of the silent killer that is sepsis.
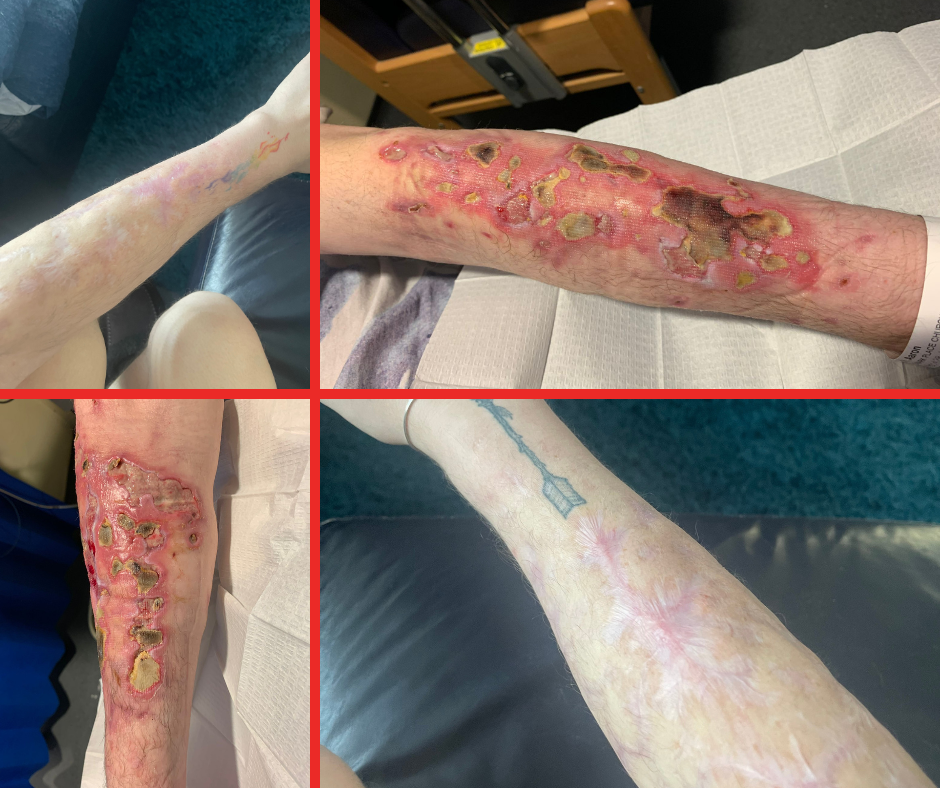
Content Note: There are photos of wounds below which some readers may find distressing
After his Diabetes diagnosis, Aaron moved to Cardiff for a fresh start, where he struggled to manage the condition due to his ADHD and depression that arose from his diagnosis. Poor management of his sugar levels led him to develop peripheral neuropathy, which caused him intense and persistent pain. Aaron said: “It feels like walking through snow barefooted 24/7; I couldn’t sleep, couldn’t work, just couldn’t function. There were days when I couldn’t walk and I would have to crawl to the bathroom.”
Initially, Aaron coped with this pain by drinking heavily. Due to his alcohol misuse, he ended up hospitalised in April 2019 with life-threatening diabetic ketoacidosis (DKA) and later found out he was treated for biliary sepsis – which left him susceptible to reinfection. After coming out of hospital, he stopped abusing alcohol but turned instead to drugs. Aaron said: “I really have to stress that this was for pain relief.
“I had never touched drugs before. It just wasn’t anything I ever thought would be part of my life.”
As his body built an ever-increasing tolerance, his drug use escalated from snorting substances to IV drug consumption as he chased that initial relief he had first experienced. “It became a case of needing more and more extreme ways in which to get that fix and relief,” said Aaron. “But it got to a point that because my veins all over my body had collapsed, I ended up injecting into just the skin, which led to numerous bouts of cellulitis in my arms and my legs.”
In an extremely low state, Aaron started picking some of the wounds on his arms, which led him to develop sepsis for a second time in July 2020. He was living alone and was drifting in and out of consciousness. After a week of being bedbound, he was able to text his sister who came to see him with her partner, who was an emergency responder and immediately suspected sepsis. Concerned for his wellbeing, his sister went to Aaron’s GP to get help, including antibiotics. Aaron said: “I found out that apparently at the time the GP told my sister, ‘If he doesn’t go to hospital, he will die’.”
Aaron’s sister and her partner called an ambulance, and he was taken to hospital – medics said they had found him during the golden hour – and treated with antibiotics; but his sepsis recovery was made all the more complicated by the drug withdrawal side effects he experienced.
After returning home, and a month of not using, Aaron returned to Cardiff, but relapsed after getting some bad news from work. Between July and his next bout of sepsis, he went into DKA again – a complication of diabetes that causes extreme thirst, frequent urination, fatigue, vomiting, organ failure and eventually, death – about four or five times but he never called an ambulance. Aaron said: “I just tried to bring myself back to a normal sugar level range to try and rescue myself. But eventually, it got to the stage again where I was bedbound for a week and I couldn’t move; I was in a terrible, terrible way. I knew sepsis was setting in again. I remember hallucinating, including a very vivid and intense feeling that I was going to die,”
Eventually, Aaron managed to contact his mum and told her to call an ambulance. Medics once again told him that if he’d left it any later to seek help, he would have died. Aaron said: “This time sepsis had started in my leg, again arising from an infected cellulitis wound. And you could see it because it was swollen and bright red.”
In early December 2020, he spent another two weeks in hospital being treated, needing surgery to put in a central line to administer antibiotics due to the state of his veins from the drug use. Again, he suffered from significant withdrawal symptoms as well as the effects of sepsis. Aaron said: “I remember that feeling of, ‘Yeah, I’m going to die’. I’d come to accept it. I wasn’t bothered, I just wanted the pain to end. Frankly, it wasn’t a case of being suicidal. It was a case of ‘I just can’t cope anymore’.”
While he’d been offered support to quit drugs by University Hospital of Wales after his second admission for sepsis, it wasn’t until the third bout of sepsis that he was finally prepared to accept it. Aaron said: “One of the team was a former user himself, and he came round and spoke to me and that made a really big difference because he was not judgmental at all, and he could understand where I was coming from. He wasn’t just saying ‘don’t do it because it’s bad’. He got it.”
Now clean for over 2.5 years, Aaron has returned to working in an organisation that he loves, where he feels truly supported by his bosses – for example, they provided a parking spot so Aaron doesn’t have to rely on public transport, which helps significantly with day-to-day pain management, along with other accommodations that help Aaron manage his various conditions. Their support extended to encouraging him to share his story with UK Sepsis Trust (UKST).
But after returning to work in August 2021, Aaron still didn’t feel quite right. He said:
“I had never heard of Post Sepsis Syndrome. I had no idea that recovery could take so long, be so much more difficult.”
“It’s almost like having a second chronic disease like diabetes; for months afterwards, I was exhausted. I just could barely move, get up. I just wanted to sleep all the time. Doing little things took huge amounts of energy and effort, going up and down stairs, going to the toilet, you know, not to mention the brain fog. And I I’m still not quite right. I don’t feel as ‘quick’ as I used to be. I feel like I stumble or stutter a lot more than I used to, or that I find it hard to get my words out.”
He also experienced traumatic psychological side effects from his experiences, including Post Traumatic Stress Disorder (PTSD), which would eventually lead him to reach out to the UKST for support. He joined a support call. Aaron said: “It just made a huge difference, coming across this whole community of people that have been through such a similar experience, and finding out that Post Sepsis Syndrome is a real thing.”
Now, Aaron actively volunteers and uses his experience to help others who have had sepsis, helping facilitate UKST online support groups or contributing to the Facebook support group. He said:
“What I really like about the online recovery support groups is just how relaxed and laid back it is. It’s very informal. There’s no pressure.”
“The facilitators of the session are always so friendly, welcoming, and it’s just a very natural flow and people are welcome to sit there and say nothing, they don’t have to have their camera on. It’s totally private.”
It was only after reading his hospital notes following a suggestion from someone else on the support group that Aaron came to learn that he had been treated for sepsis when he was first admitted in April 2019. Recently, Aaron was diagnosed with Fibromyalgia and Chronic Fatigue Syndrome (CFS), which he understands are a direct result of having had sepsis and glandular fever (which he didn’t know he had had, until his hospital admission in April 2019, where blood work showed he had had it at least several weeks prior to admission).
Throughout everything that happened to him, Aaron’s family have been by his side. “I can’t thank my praise or thank my family enough. I’m so lucky that I had them,” said Aaron.
“I wish I could speak to my previous self, tell them to stop because it doesn’t make it any better. You’re just making the pain worse. You’re hurting your family, it’s not worth it.”
“It’s not worth putting yourself through sepsis. If I could tell my previous self to do anything to avoid getting sepsis, I would.”
His experience has given him a greater understanding of and sympathy for the manifold reasons that people turn to drink and drugs in the first place. While he would do anything to turn back the clock himself, ultimately he has learned not to make assumptions about others. Aaron said: “A silver lining is that I’ve learned you can’t judge people without knowing their story.”