Rachel Stuart is a Type 1 diabetic, and was also diagnosed with Chronic Kidney Disease in January 2022. She was aware of the signs of sepsis, having had it before. But last year, she arrived at A&E in the nick of time…
She’s sharing her story now in the run up to Diabetes Week (12th-18th June) to help make others aware of what to look out for, to help save lives.
In February 2022, Rachel woke up with pain around her kidneys. Initially, she didn’t think too much of it as she is used to feeling poorly. But she rapidly went downhill over the next two hours. She said: “I went downstairs to get some pain relief and a hot water bottle before jumping back into bed. But it just got worse very, very quickly. And my partner was quite insistent that I went to the hospital. By the time I got to the desk at the A&E I collapsed on the floor.”
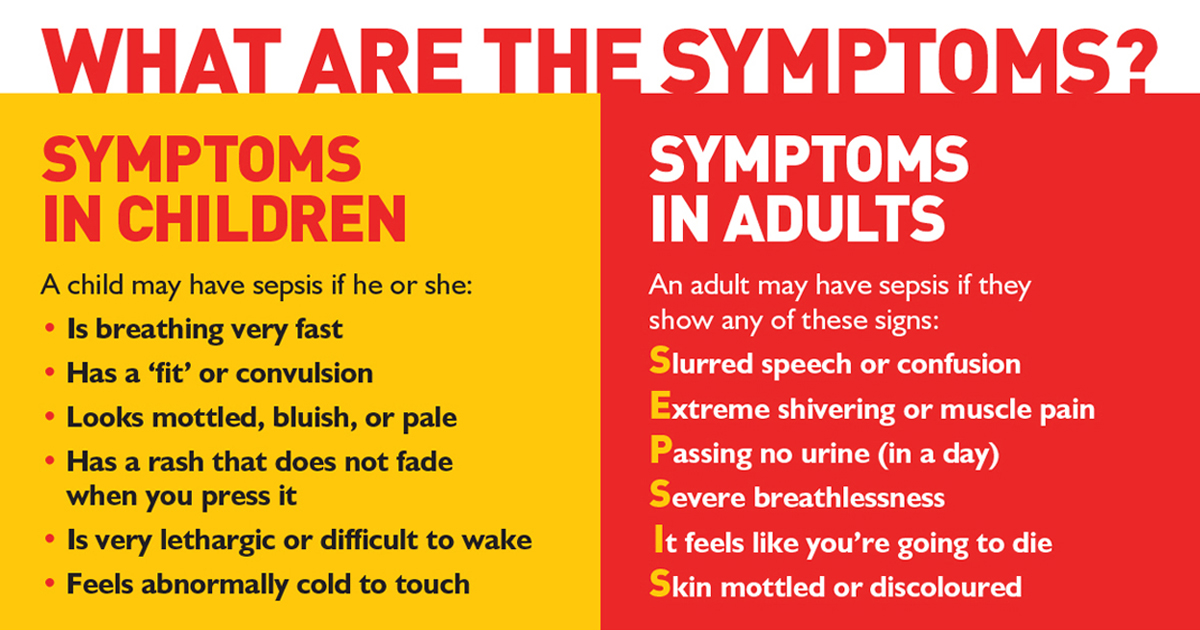
Rachel had had sepsis before, so was insistent on telling the doctors and nurses that it felt like that, because she understood time was of the essence. Rachel was also exhibiting several of the key signs of sepsis. She said: “I just felt really awful. I was shivering, I felt freezing cold, but I had a really high temperature. I was vomiting and I felt really breathless. I felt I couldn’t breathe properly. And I just felt this sort of overwhelming feeling, not so much that I felt like I was going to die, but it felt like I knew that it was bad.
“Within a couple of hours, I couldn’t look after myself, wasn’t capable of being stood up and holding a conversation. It just wasn’t right at all.”
Eventually, Rachel went into septic shock in A&E, and staff struggled to keep her blood pressure up. She was moved to intensive care, where she stayed for two and a half weeks, before being transferred to the specialist kidney unit where she was treated for a further three weeks before being allowed to go home.
Her time in ICU was particularly traumatic, as Covid restrictions meant that she wasn’t allowed to have loved ones around her. Rachel said: “The doctors and nurses were incredible, but there’s only so much you can get out of a phone conversation with a professional; if it’s your loved one, you want to be able to see them with your own eyes and be there with them. There were a lot of things that happened that were incredibly scary or painful and having someone else there for that would’ve made it easier.”

Leaving hospital, Rachel experienced flashbacks and issues regulating her emotions. She found out about Post Sepsis Syndrome through UKST, and found comfort in the knowledge that a lot of what she was experiencing was common among sepsis survivors. She said:
“I read all the information and before I didn’t realise that hair loss could be related to sepsis.”
“And having things like brain fog, when you’re having conversations, and you feel like words aren’t coming out as they normally would – reading about that was reassuring because it meant that I wasn’t losing my mind, which was quite nice.”
Eventually, Rachel was able to access counselling through Kidney Care UK to help her process what happened to her while she was in ITU, and she even revisited the intensive care unit where she had been treated, where staff helped to create a journal to help her come to terms with gaps in her memory. But a year on from her hospitalisation, Rachel feels like she is still on her recovery journey. She said: “It took a while to get back to where I was physically. To be fair, I would probably say that I’m still not there. I don’t know whether I will be able to get back to the levels of fitness that I had before.”
Having managed her diabetes since she was a child, Rachel was perhaps more aware of her risk of infection and therefore sepsis than others. She said:
“I think for type one diabetics, it’s important to understand that when you have an infection, you can become more poorly and poorly faster than your average person because your immune system just isn’t on the same level as with someone without diabetes.”
She has chosen to share her story with UKST in June 2023, in the run up to Diabetes Week. Rachel encourages others to go to the doctor if you have concerns, rather than sitting on worries. She said: “Sometimes I’m still guilty of it now, where I think, ‘Oh, I won’t bother the doctor with that, I won’t bother them with X, Y and Z’. But it can save your life if you do make that call or seek that support and that is definitely something I’ve taken away from this.”