Clinical Tools
On this page you can access our free operational clinical tools, which have been updated following revisions to the National Institute for Clinical Excellence’s NG51 sepsis guideline made in January 2024.
NICE aligned tools and resources
On the 31st of January 2024, NICE updated its NG51 guideline for the UK originally published in 2016. The updates predominantly centred around the use of the National Early Warning Score (NEWS2) and recommendations around the timing of antibiotics made by the Academy of Medical Royal Colleges in 2022.
Updated for 2024 and designed by our panel of expert clinicians in consultation with NICE, our new suite of clinical tools reflects the latest updates to NG51 and can now be implemented into clinical practice across the spectrum of healthcare. They aim to provide the optimum balance between saving lives from sepsis and a responsible approach to antimicrobial stewardship.
Dental Primary Care Women Who are Pregnant or up to 4 Weeks Post-Partum
Read moreDental Primary Care 16+
Read moreDental Primary Care 12-15
Read moreDental Primary Care 5-11
Read moreDental Primary Care Children Under 5
Read moreOut of Hours (OOH)/ Telephone Triage Women Who are Pregnant or up to 4 Weeks Post-Partum
Read moreOut of Hours (OOH)/ Telephone Triage 16+
Read moreOut of Hours (OOH)/ Telephone Triage 12-15
Read moreOut of Hours (OOH)/ Telephone Triage 5-11
Read moreOut of Hours (OOH)/ Telephone Triage Children Under 5
Read moreGeneral Practice Women Who are Pregnant or up to 4 Weeks Post-Partum
Read moreGeneral Practice 16+
Read moreGeneral Practice 12-15
Read moreGeneral Practice 5-11
Read moreGeneral Practice Child Under 5
Read moreAmbulance Services Women Who are Pregnant or up to 4 Weeks Post-Partum
Read moreAmbulance Services 16+
Read moreAmbulance Services 12-15
Read moreAmbulance Services 5-11
Read moreAmbulance Services Children Under 5
Read moreCommunity Services Women Who are Pregnant or up to 4 Weeks Post-Partum
Read moreCommunity Services 16+
Read moreCommunity Services 12-15
Read moreCommunity Services 5-11
Read moreCommunity Services Children Under 5
Read moreAcute Mental Health Facilities
Read moreAcute Hospital Women Who are Pregnant or up to 4 Weeks Post-Partum
Read moreAcute Hospital 16+
Read moreAcute Hospital 12-15
Read moreAcute Hospital 5-11
Read moreAcute Hospital Children Under 5
Read morenon-NICE approved tools & resources
For organisations that have implemeted or are piloting the new National Paediatric Early Warning Score (PEWS), or the National Maternal Early Warning Score (MEWS), please select the tools suitable for use from the list below.
National PEWS Community Tool
Read moreNational MEWS Tool
Read moreNational PEWS Tool
Read morePaediatric Hospice Care 12+
Read morePaediatric Hospice Care 5-11
Read morePaediatric Hospice Care Children Under 5
Read moreMarie Curie End of Life Community Setting
Read moreMarie Curie Hospice Setting
Read more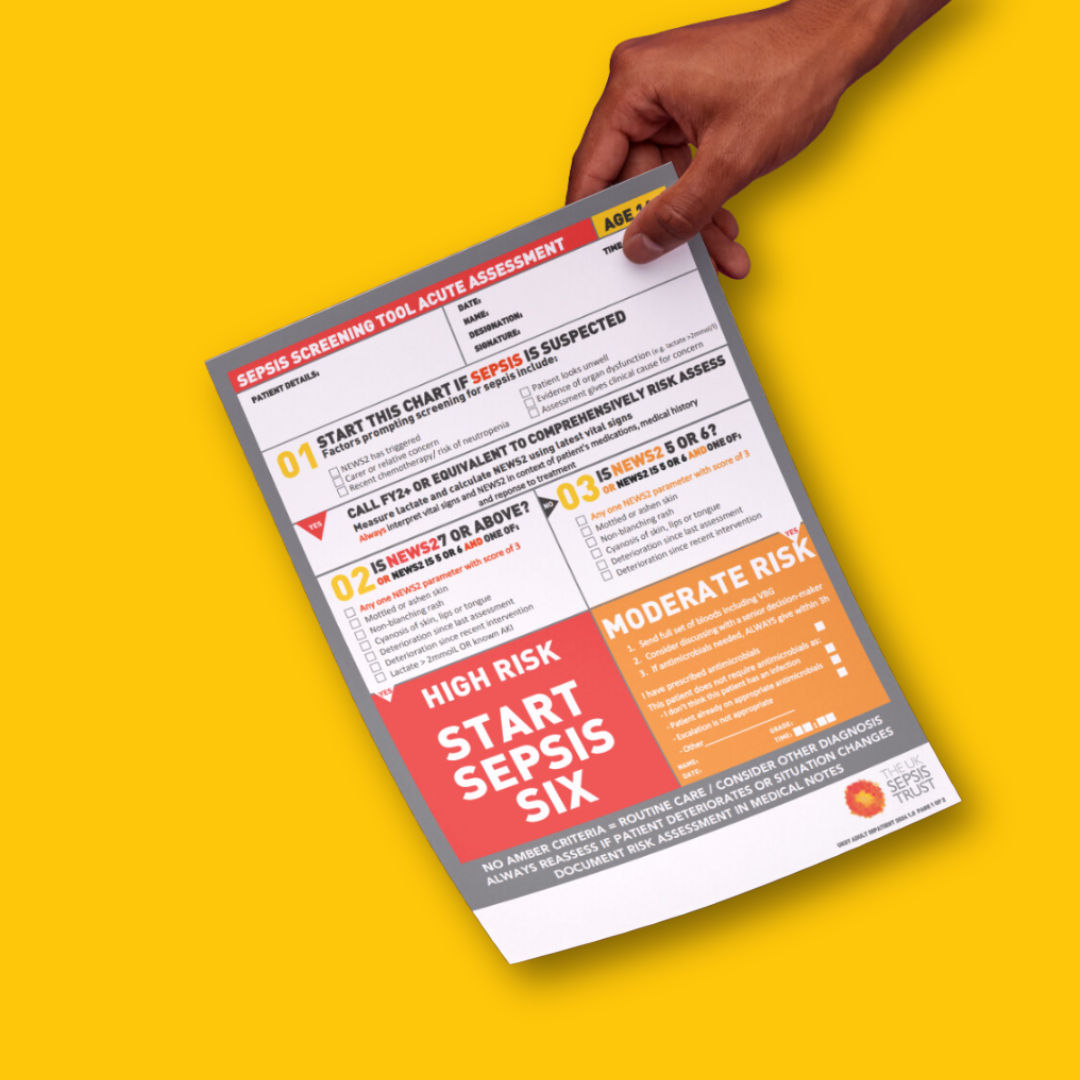
Customise our clinical tools
You can use our tools as they are, or customise with your organisation logo/site name upon download, but if you require any further modifications then please get in touch with us first: melissa@sepsistrust.org
We recommend you sign up for updates, so that we can let you know when the tools are updated. You can just download the tools, but in that case, we recommend you regularly revisit our site to check if there have been any changes.
Thank you for your cooperation! This process helps us keep patient safety at the forefront of our work in the clinical space.
About our tools
Since 2015, the UK Sepsis Trust has collaborated with a number of organisations to produce operational clinical tools for all ages (except specifically for neonates) across a wide range of healthcare settings.
On the 31st of January 2024, NICE updated its NG51 guideline for the UK originally published in 2016. The updates predominantly centred around the use of the National Early Warning Score (NEWS2) and recommendations around the timing of antibiotics made by the Academy of Medical Royal Colleges in 2022.
Updated for 2024 and designed by our panel of expert clinicians in consultation with NICE, our new suite of clinical tools reflects the latest updates to NG51 and can now be implemented into clinical practice across the spectrum of healthcare.
They aim to provide the optimum balance between saving lives from sepsis and a responsible approach to antimicrobial stewardship. These new tools can be used alongside our additional resources and e-learning programme.

More from UK Sepsis Trust
Get Sepsis Savvy
Knowing the signs of sepsis can help save lives. Test the knowledge you’ve acquired on this page by watching a short video and playing our game.
Sepsis support
If you or someone you love has been affected by sepsis, our trained Support Nurses are here for you.
Order sepsis resources
We have a range of sepsis resources including posters and leaflets that you can order via our shop and display to help raise awareness of this silent killer.